Have any questions?
+44 1234 567 890
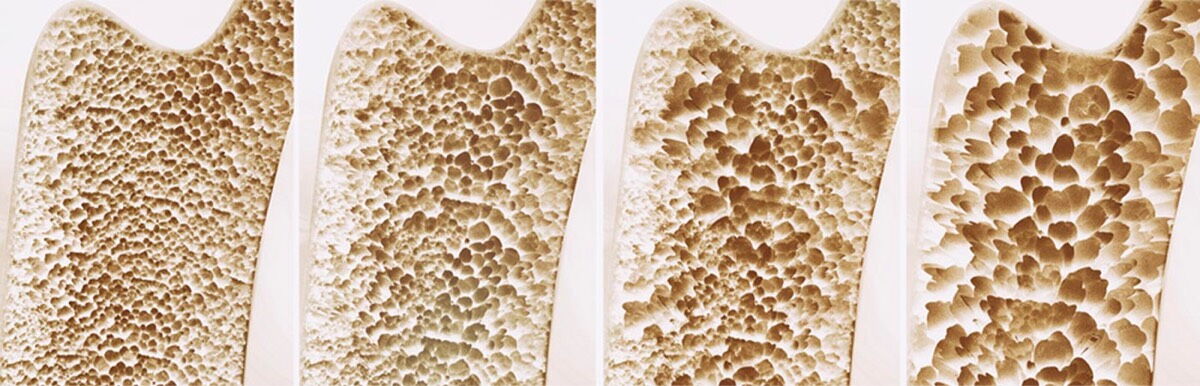
As part of the normal ageing process our bones lose density. However, when this decrease in bone strength and density is significant (usually due to certain additional risk factors), too much bone substance may be lost, causing osteoporosis to develop. Osteoporosis is a condition which causes bones to weaken and make them more likely to fracture easily.
This decrease in density does not happen overnight, so many patients do not recognise the time when they need to take action. By taking an OsteoTest you can find out the status of your bone health and identify your risk of developing osteoporosis, enabling you to take any necessary steps to support your bone health before it's too late.
The stage before osteoporosis is called osteopenia and this is where your bone density is lower than the average for your age but not sufficiently low enough to be classed as osteoporosis. Unfortunately, osteoporosis cannot yet be cured. However, with awareness and the right bone health management, you can delay or prevent the disease from developing in the first place. Timely treatment, in turn, can slow down the progression of the disease and prevent further complications.
Who is affected?
It is estimated that over 3 million people in the UK currently suffer from osteoporosis and over 500,000 will receive hospital treatment for fragility fractures. Osteoporosis usually occurs in those over the age of 50 years, and is more common in women than men, typically one in three women will suffer with the disease and one in five men.


Causes and risk factors
Osteoporosis can have different causes and be triggered by different factors. Hormones are to blame for brittle bones in about 70 percent of cases. As the production of oestrogen decreases in women during the menopause, this has a negative effect on bone metabolism, because the oestrogens inhibit the cells that break down bone. The balance of bone breakdown and bone formation that regenerates healthy bone is tipped and more bone mass is lost. Women who had their first period relatively late as teenagers or went into the menopause very early are particularly at risk for osteoporosis. Women who have not had children or whose ovaries have been removed are also at increased risk of osteoporosis.
In 30 percent of cases, osteoporosis develops as a secondary disease of another (long-term) illness such as asthma, hyperthyroidism, kidney problems or chronic inflammatory bowel disease.
Other risk factors include having a family history of fractures, being underweight, having a poor diet, lack of exercise, alcohol, smoking and excessive consumption of fizzy drinks.
It is much more sensible to check the risk of osteoporosis when entering the menopause rather than waiting for warning signs. The earlier a dangerous decrease in bone density can be diagnosed, the greater the chances of reducing the risk of disease with therapy and preventative measures.
What are the symptoms of osteoporosis?
Osteoporosis usually develops slowly over time, at first, those affected may not even be aware they have the condition. This is why it is often called “The Silent Disease”. Diagnosis is often not made until it has reached an advanced stage. Nevertheless, there are a few possible warning signs.
- Acute and chronic back pain
- A fracture caused by a slight movement or low impact fall
- Joint pain
- Loss of height over time
- An increasing stooped posture


How is osteoporosis detected?
Traditionally osteoporosis is diagnosed with the help of an X-ray image, unknown as a DXA scan. The scan is used to measure bone density. Images are taken of both the hip and base of the spine and your bone density is compared to that of a healthy young adult. On a DXA scan, the result of the bone density measurement is given as a so-called T-score.
In addition to a DXA scan a Doctor might calculate your risk of fracture using an online fracture risk assessment calculator giving you an indication of the percentage likelihood of you suffering a fracture in a 10 year period.
Unfortunately osteoporosis is often undetected until the disease has already progressed as there is no screening programme in place. A DXA scan is not usually requested until a fracture (or even multiple fractures) has occurred and osteoporosis does not show up on an X-ray until significant deterioration has occurred.
Ways to help prevent osteoporosis and support your bone health
There are many lifestyle measures that you can take to help support your bone health to try and prevent osteoporosis developing, or slow down the progression the disease. For example;
- Eating a varied and well balanced diet, including calcium and Vitamin D
- Muscle strengthening exercises such as yoga, pilates and weight training to help support the skeleton
- Weight bearing sports, the higher impact the better eg: walking, jogging, racket sports, dance)
- Cutting down on alcohol and smoking
- Maintaining a healthy balanced weight
- Taking oestrogen if this is suitable
- Try to take steps to minimise the risk of falls eg; remove loose rugs and other slipping or tripping hazards


Possible treatment approaches
If you have been diagnosed with osteoporosis, your doctor will recommend the best treatment for you. Depending upon the severity of your bone loss, you may be prescribed medication.
Bisphosphonates are the most common group of osteoporosis drugs. There are complex differentiations in effect, combination and administration as well as different active substances within the group.
The main effect of bisphosphonates is to inhibit the activity of cells that break down bone. The resulting natural reconstruction of healthy bone tissue leads to an increase in bone mass and fewer bone fractures. Bisphosphonates are available in the form of tablets (taken daily, weekly or monthly), as an injection or infusion solution. Treatment duration will vary and success will be reviewed by repeating a DXA scan.
Patients with only a slightly increased risk of bone fractures or only a slightly reduced bone density (osteopenia), may feel it is worth weighing up the advantages and disadvantages of treatment with medication and first try conservative therapy with more exercise and a healthy osteoporosis diet.
Further information
For more information about osteoporosis, including risk factors, diagnosis, treatment and life style measures that can be taken, as well as support for those who have been diagnosed, we recommend that you visit The Royal Osteoporosis Society.
Information can also be found on the NHS website.